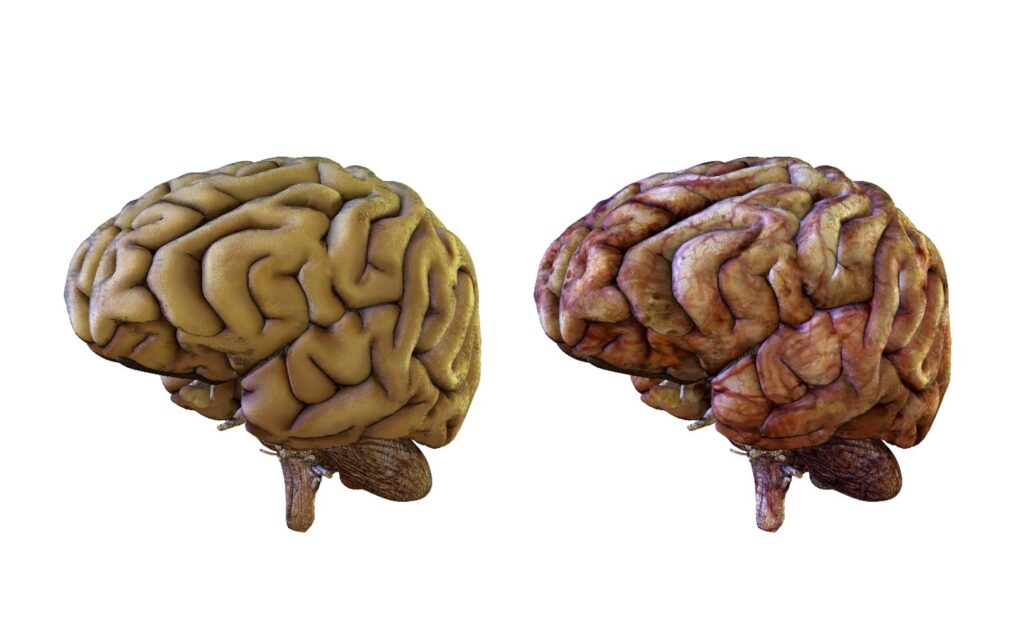
Brain deterioration can occur as a result of several disease-based processes, including some cancers, traumatic brain injuries, and cognitive impairments such as Alzheimer’s disease and dementia.
Whatever the cause, many millions of individuals each year develop some aspect of brain deterioration. It’s seen over time in many individuals, and the elderly are at higher risk of this process developing.
While in some cases, brain deterioration is progressive and slow-moving, other cases, such as those related to cognitive impairments, may seem to have developed spontaneously.
In what follows, we’ll be exploring the most common signs of brain deterioration, particularly concerning the clinical features of post-stroke patients and patients with vascular dementia.
What Occurs In Brain Deterioration?
Inside the human brain are billions of nerve cells called neurons. Neurons communicate with each other via chemical signals known as neurotransmitters. These neurotransmitter molecules travel along the neuron’s long extensions called axons, where they bind to receptors located on adjacent neurons. This process allows one neuron to send a signal to another. In addition, neurons receive information from other cells via synapses. When a neuron receives a signal, it changes its electrical activity; this change is transmitted down the axon to the next neuron.
The weight and volume of the brain decrease by about 5% every ten years after age 40. This is due to the atrophy of both grey matter and white matter. It is thought that the rate of decrease increases with age. However, it is possible that these changes can accelerate later in life.
The levels of the neurotransmitters dopamine and serotonin change dramatically in the aging brain. Dopamine levels decline by around 10% per decade from early adulthood and have been associated with declines in cognitive and motor performance. Serotonin levels also fall with increasing age and may be implicated in the regulation of the synapse unit and neurogenesis.
Brain deterioration is seen in the following conditions.
Post-Stroke Dementia

Following the diagnosis of a stroke, patients may further experience signs of cognitive decline and impairments. These further declines are defined as post-stroke dementia and are characterized by brain deterioration.
Certain medical conditions can increase the risk of post-stroke dementia. Some of these risk factors include:
- Age
- Diabetes
- Atrial Fibrillation
- Intracerebral Hemorrhage
Signs of post-stroke dementia include confusion, short attention span, difficulty processing information, seizures, and memory loss. Additional signs include difficulty maintaining balance, loss of vision, mental and physical fatigue, and alterations of speech.
Though not seen in all individuals, the most common characteristic of post-stroke dementia is impairment of executive function and memory.
Vascular Dementia
Unlike brain deterioration which is seen soon after a stroke, vascular dementia is characterized by a progression of brain deterioration over time that occurs without any history of stroke.
This progression of signs and symptoms can develop rapidly or at a stepwise slower pace.
The risk factors associated with vascular dementia are similar to those associated with a stroke. Such risk factors include age, lifestyle, obesity, diabetes, hypertension, and heart disease.
Common signs of vascular dementia include progressive confusion, loss of attention and focus, memory loss, lack of steady gait, impaired ability to organize thoughts, and depression. In addition, individuals can become quite emotional and have unexplained crying episodes.
Preventing Brain Deterioration
Many causes and risk factors are associated with both post-stroke dementia and vascular dementia. Yet, several steps can be taken to attempt to mitigate or prevent the development of the condition.
Certainly, the development of dementia and other related signs of brain deterioration can’t always be prevented or reversed. Still, a common theme of prioritizing lifestyle is the best way to decrease overall risk.
The following are some key decisions that will improve general health and brain health and protect the brain’s blood vessels, thus reducing the likelihood of brain deterioration.
Exercise Regularly – Not only will regular exercise promote weight loss and reduce the risk of obesity, but it will also promote healthier blood pressure and heart function, which are two risk factors for dementia and brain deterioration.
Quit Smoking – This awful habit is a common risk factor for several health-related conditions and diseases, including dementia and brain deterioration. Smoking causes ongoing damage to blood vessels, leading to high blood pressure, risk of clots, and impaired blood flow to the brain. By quitting this habit, you immediately stop damaging blood vessels, allowing them to heal, repair, and become healthy again.
Eat Healthily – A healthy diet will promote healthy triglyceride levels while reducing the likelihood of obesity and weight gain, thus reducing the risk of stroke and other conditions leading to brain deterioration.

Final Thoughts
Post-stroke dementia and vascular dementia are hallmarks seen in individuals with brain deterioration, resulting in a decreased quality of life.
Efforts to live a healthy lifestyle have the potential to make a big difference in decreasing the risk of brain deterioration.
