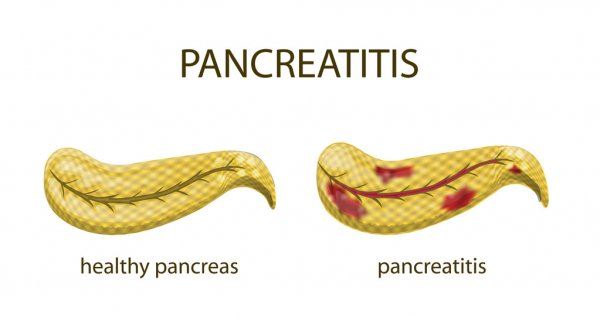
Inflammation of the pancreas is known as pancreatitis. This condition occurs because digestive enzymes in your body, which usually work to break down food, begin accumulating in the pancreas and digesting the tissues there. This causes inflammation and pain, and it can often be very dangerous.
Pancreatitis can be either acute or chronic. In either case, it often requires hospitalization, so it’s important to take care of your gastrointestinal health so you can reduce your risk of developing this condition.
Symptoms of Gastrointestinal Health Issues
The symptoms of pancreatitis are common to many kinds of gastrointestinal health conditions that can cause stomach upset and digestive distress. Abdominal pain of any kind is a sign that there may be something wrong in your digestive tract, so it’s important to have any excessive or persistent pain checked out by a doctor as soon as possible.
Early detection and treatment of gastrointestinal issues can greatly limit how much damage they do to your body. This allows you to avoid pancreatitis or manage the condition if you develop it.
Note that symptoms for acute and chronic pancreatitis can differ slightly, with acute symptoms coming on quickly, while chronic symptoms may be less noticeable and therefore downplayed.
Acute Pancreatitis Symptoms

Acute pancreatitis typically involves rapid onset symptoms and more significant pain than its chronic counterpart. This pain typically occurs in the upper abdominal region, though it may spread to your back, and the discomfort is often worse after a meal. It can cause tenderness if you press on your abdomen.
You may also experience nausea, vomiting, indigestion, sweating, fever, and a sharp increase in your pulse.
These symptoms indicate an inflamed pancreas, which will likely require treatment at a hospital.
Chronic Pancreatitis Symptoms
In addition to the acute symptoms, which can occur during flare-ups, symptoms of chronic pancreatitis include unexplained weight loss and stools that are unusually malodorous or oily.
Chronic pancreatitis can result in the development of several long-term health effects such as scarring of the pancreas and damage to the cells that produce insulin, raising your risk of diabetes.
Causes of Pancreatitis
Pancreatitis has been linked to multiple gastrointestinal conditions, lifestyle choices, and other health conditions that inflame the pancreas.
Gallstones
According to the National Pancreatitis Foundation, gallstones are the most common cause of acute pancreatitis. Gallstones, which are formed in the gallbladder, can actually pass into the pancreatic duct and cause obstruction, keeping pancreatic enzymes trapped inside the organ. This causes irritation and inflammation.

Alcohol Consumption
Most people who drink in moderation do not have any issues with their pancreas, but those who drink excessively may be at a higher risk of developing pancreatitis. Typically, your chances of developing this condition increase if you have four or more drinks per day on a regular basis.
Gastric Conditions
Conditions like Crohn’s disease and ulcerative colitis have also been correlated with a higher risk of acute or chronic pancreatitis. Managing these conditions through adopting healthy habits is a great way to prevent pancreas issues.
Pancreatitis and Gastrointestinal Treatments
Pancreatitis flare-ups are generally severe enough that they warrant professional medical attention.
Once your doctor considers your condition to be stable, they will help you find a treatment method that works for you. Treatments typically involve adjustments to your diet, medications, and risk factor management.
Dietary Changes
While your pancreas recovers, you may need to fast for a few days and follow a bland or liquid diet before you can return to your regular eating habits. It’s best to stick to a low-fat diet as well, as it is easier for your body to process and puts less strain on your pancreas.
Gastrointestinal Medicine
Common medications used to treat or manage pancreatitis include pain medications and pancreatic enzyme supplements. Pancreatic enzymes can be taken with every meal to help your body break down food more efficiently, improving your nutrient intake. This helps your body be less dependent on a pancreas that may be somewhat compromised by this condition.
Reducing Risk Factors
If your case of pancreatitis is linked to other health issues like gallstones or heavy drinking, it’s important to manage these risk factors so they don’t cause future flare-ups. Cut back on alcohol, limit fatty foods known to cause gallstones, and speak with your doctor about any potential surgical options, such as removal of the gallbladder.
Final Thoughts
Avoiding pancreatitis and managing chronic symptoms involves addressing key factors that contribute to gastric health and your overall wellbeing. Take care of yourself by addressing the root causes of the condition and seeking treatment when necessary.
