Diabetes has become a global epidemic, affecting 422 million people, an increase from 100 million 24 years ago. With this trajectory, it’s become clear that developing a cure is a high priority.
The biotech industry is making tremendous strides, especially for type one diabetes (T1D). Type two diabetes (T2D) is also concerning because it comes with many potential complications if poorly managed.
Recent advancements in the industry have improved the ability to monitor this condition much better, and other research is very promising for the future.
Let’s take a look at these exciting advancements.

Diabetic Monitoring Advancements
As science and technology stride forward in the war against diabetes, glucose monitoring continues to improve.
The first product being developed is called the smart contact lens. Jihun Park and his colleagues at the Ulsan National Institute of Science and Technology in South Korea have already created a prototype.

The lens looks like a regular contact lens, and it’s designed for comfort. As soon as your glucose levels spike, the lens switches over to light emitting diode (LED) mode, which allows you to read your glucose levels in a mirror.
Another non-invasive monitoring method is adding special ink to tattoos. Created at the Massachusetts Institute of Technology (MIT) and Harvard, the color-changing ink turns brown when your glucose levels spike.
The pleasant point about these ideas is that they offer ways to monitor your glucose levels without pricking your fingers. Another non-invasive monitor includes a graphene patch that monitors hair follicles.
The needle-free monitoring revolution has begun, but challenges still need to be overcome.
Lexicon Inhibitor Trials
Another therapeutic approach is under investigation in T1D, and more research might make this a viable option for T2D. Lexicon Pharmaceuticals has run successful trials of a new drug called LX4211.
This drug targets the sodium-glucose transporter 1 (SGLT1) in the digestive tract, which absorbs glucose from the bloodstream. It also targets the SGLT cells surrounding the kidneys, which are responsible for reabsorbing glucose.
This scientific trial studied patients with T1D taking a 400mg dose of the drug over a 30 day period. The drug was effective in allowing the patients to excrete the excess glucose by the kidneys.
Previously, this drug had shown the ability to increase certain hormones that improve glycemic index and appetite in patients. The plan is to expand the trials and examine how successful this drug can be in T2D as well.
Targeted Immunotherapy
Immunotherapy is another advancement in treating T1D. Recall that T1D is caused by the autoimmune phenomenon where the immune cells attack insulin-producing cells. Belgian biotech Imcyse had some success in phase one of their trials with immunotherapy.
It’s estimated that newly diagnosed T1D patients still have up to 10% of their original beta cells for three to six months after the T1D diagnosis is first made. Imcyse took 41 recently diagnosed patients and conducted a trial on targeted immune cell eradication.
The trial lasted six months, and the drug proved effective in eliminating the autoimmune cells responsible for destroying the beta cells in the pancreas.
This result has been a great success, but a key requirement for the immunotherapy to work is that patients get started with therapy as soon as possible after diagnosis. Otherwise, the pancreatic beta cells will already be destroyed by the disease.
Diabetic Vaccines
Professor Bart Roep from the Department of Diabetes Immunology is working on a vaccine intended to correct the immune system in T1D patients before it destroys too many pancreatic B cells to prevent the onset of T1D.
With this method, you are attempting to stop the autoimmune problem before it even begins. In the process, blood is taken from the patient, and white blood cells are isolated to create dendritic cells.
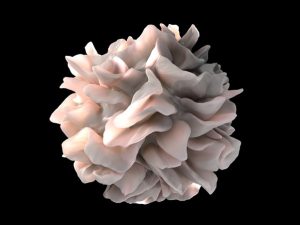
Dendritic cells train other immune cells like T-cells to recognize that pancreatic beta cells are not real pathogens and shouldn’t be attacked.
The dendritic cells are then grown in a lab for six days in a solution with vitamin D so that they become anti-inflammatory, which improves their function.
Then they are treated in a proinsulin solution to build a tolerance. Proinsulin is an autoantigen protein that normally destroys beta cells. This is how the training takes place before you receive the vaccine.
The dendritic cells train the T-cells not to destroy the insulin-producing cells, and these trained cells then become regulatory T-cells, which prevent other immune cells from attacking your pancreas.
The vaccine is administered by a patch, which is placed on the abdomen where your pancreas lies. The patch has many microneedles that inject the trained immune cells into the body, where they make their way into the pancreas.
The first study was conducted on nine patients with T1D who continued their insulin treatments for six months while also using the patches. The results showed no further damage to the pancreatic beta cells. These are very promising results warranting further study.
Final Thoughts
The work being done in science and technology is bringing us closer to a cure for diabetes. From non-invasive monitoring to vaccines, we’re taking steps closer. There is hope to find more advancements in this debilitating disease.
