Some advancements in research have potentially brought us closer to the goal of finding a cure or better method of treating type one (T1D) and type two diabetes (T2D).
Both conditions can lead to serious complications. Let’s see what further developments are undergoing research now.

The Mexican Cavefish
What does a fish have to do with diabetes? This chubby, blind cave-dweller has evolved to be insulin resistant. Intrigue abounds when comparing the cave-dweller to its river-dwelling counterpart from the same species.
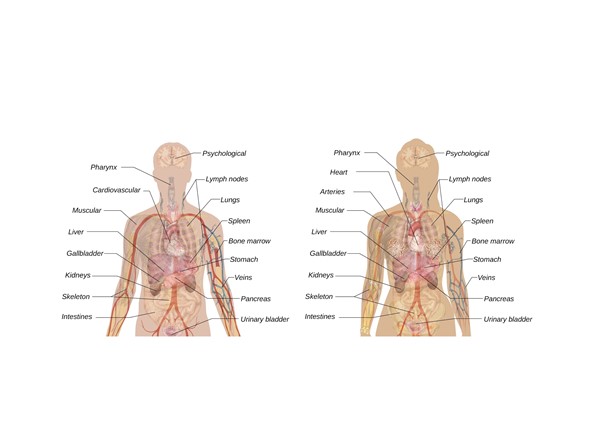
Insulin is released from the pancreatic B cells after eating, and this regulatory hormone latches onto receptors in your muscles, liver, and fat. Insulin absorbs the glucose from carbohydrates in the bloodstream into the cells.
Your blood glucose levels normalize, and some glucose is burned for energy while some is stored as glycogen for later use. When your body starves, the pancreas releases glucagon, which converts glycogen back to glucose for energy.
Biologist Misty Riddle from the Stowers Institute for Medical Research examined the cave-dwelling fish closely to understand how it survived in its environment if it was insulin resistant.
The cave-dwellers glucose levels were up and down after eating and fasting for 21-days, much more so than the river-dwelling fish. The cave-dwelling fish converted their proline amino acids to leucine amino acids, a phenomenon seen in cases of severe insulin resistance.

These fish have evolved to be diabetic, but they’re also living longer than the river-dwelling fish, confirming that they’ve adopted alternative mechanisms to thrive even in their diabetic state.
The Mexican cavefish phenomenon provides a means to investigate how T2D patients could adapt their natural homeostasis and avoid complications of their underlying diabetes.
The Microbiome
The microbiome is the collection of bacteria that protects your stomach, and it has a role in hormone regulation and the immune system. Imbalances in this gut flora can be a source of problems in managing diabetes.
Trials are currently underway to enhance the flora and add a variety of bacteria that could help diabetics restore gut flora imbalances.
Virgin Beta Cells
Islet transplant therapy is when clusters of pancreatic cells from donors are transplanted into diabetic patients so that they can produce insulin again.
During recent research, astonishing evidence was found of a new type of cell in the pancreatic islets clusters, which are the cells attacked and depleted in T1D.
Among the clusters were immature beta cells, also called “virgin beta cells.” The question was whether these previously unnoticed cells could be matured to function as insulin-producing cells.
Mark Huising from the University of California and his colleagues are currently researching the virgin cells to determine whether they can be matured to respond to glucose levels in the bloodstream and release the necessary insulin.
The immature beta cells lack the receptors to determine blood glucose levels. Further research will be needed to determine if these cells can subsequently develop these receptors and become fully functional.
Artificial Pancreas
A few different types of artificial pancreas exist today. Insulin pumps and the apps that work with them help parents monitor and care for children with T1D. The apps monitor glucose levels, and the pump automatically injects the right dose.
The concept of the artificial pancreas is to replace the organ with newly placed virgin beta cells that are manipulated to prevent the immune system from attacking them.
Researchers are still faced with two of the biggest problems: The scarcity of donors making it hard to conduct human trials and overcoming the immune system response to the virgin beta cells.
However, a new bioengineered pancreas was tested in a different body location, and the results from one woman’s improved T1D showed some success. The female T1D patient had the artificial organ transplanted into her omentum, and she had improvement of her T1D.
The omentum is a large, flat tissue made of a fatty membrane in front of the intestines. The artificial organ in that region mimicked the pancreas more successfully than other transplant sites.
Improvement in three areas will be beneficial in the advancement of the artificial pancreas:
- Faster-acting insulin.
- The use of Amylin, another hormone that improves the activity of insulin.
- Improving insulin dose algorithms.
Great strides have been made so far, but overcoming these problems will be a considerable advance in the treatment and methodology of curing T1D.
Final Thoughts
Learning from nature always helps science advance in treating chronic conditions, and the success of various therapy trials continues to grow.
There might not be a cure for diabetes today, but the future holds promise for millions of people globally.
